Healthy Heart Program
Is my Heart Healthy?
Are you making smart food choices, getting good sleep, managing stress, keeping mind and body fit? All of these things directly effect your heart health.
Are you experiencing some concerning symptoms?
- Shortness of breath during rest or physical exertion
- Visible swelling in the legs, ankles, and feet due to fluid buildup (this is called edema)
- Persistent fatigue
Heart Failure is a scary phrase, but it's something to look into if these symptoms are now a part of your day-to-day.
Heart Health Resources
What Is Heart Failure?
Heart failure occurs when the heart can’t pump enough oxygenated blood throughout the body. Although the heart continues to pump blood, it does not work as efficiently as a healthy heart. People with heart failure often are short of breath, fatigued, and cannot exert themselves. Many forms of heart disease can lead to heart failure, including coronary artery disease or chronic high blood pressure, as these conditions leave the heart progressively weaker or stiffer. The body is designed to react to sudden emergencies, such as an attack or blood loss, by activating reflexes that make the heart pump harder and faster and fill up with more fluid. These reflexes remain active when a person experiences chronic heart failure, increasing the load on the injured heart and weakening it further.
Heart failure cannot be reversed or cured. Still, ongoing treatment, including making any necessary lifestyle changes is crucial to improving your quality of life and reducing the impact of the symptoms.
Heart Failure Symptoms
Every person with heart failure experiences symptoms differently, but in general, the symptoms include:
- Shortness of breath during rest or physical exertion
- Visible swelling in the legs, ankles, and feet due to fluid buildup (this is called edema)
- Persistent fatigue
- Abdominal pain or nausea
- Loss of appetite
- Weight gain
- Wheezing
- Persistent cough, often tinged with blood
- Dizziness and confusion
If you have more than one or more symptoms of heart failure, even if you haven't been diagnosed with any heart problems, report them to your health care professional and ask for an evaluation of your heart.
Take a moment to watch our 2024 February Heart Month Series that was posted to our social media (Instagram and Facebook.) These 4 videos feature a former CHC employee and Down East resident, Myrna Willis. We just love Mrs. Myrna!
Causes of Heart Failure
Heart failure may result from a variety of heart conditions and diseases. When a specific cause of congestive heart failure is discovered, this will guide your doctor to the appropriate treatment. For instance, if you have heart failure caused by high blood pressure, then that should be treated, or if you have an abnormal heart valve, then surgical valve replacement may be necessary.
Other causes of heart failure include:
- Previous heart attack, often resulting in scar tissue that may interfere with the heart’s ability to pump effectively
- Coronary artery disease, or narrowing of the arteries
- Heart valve disease caused by infections such as past rheumatic fever
- Heart valve and/or muscle infection, such as endocarditis or myocarditis
- Heart muscle disease, such as cardiomyopathy
- Congenital heart disease or defects, present at birth
- Cardiac arrhythmias, a type of irregularity of the electrical activity of the heart that causes irregular heartbeat
- Pulmonary embolism, caused by a blood clot in the lungs
- Complications of diabetes
- And more
Heart Failure Diagnosis & Treatment
Your doctor will take a complete medical history, conduct a physical examination, and ask you about any medication you take, including anything over-the-counter or supplements. Your doctor will use a stethoscope to listen to your lungs for signs of congestion and to pick up abnormal heart sounds. Based on these results, your doctor may order blood tests to look for signs of diseases that can affect the heart. A chest X-ray will be ordered to assess the condition of your lungs and heart. Further testing, such as an electrocardiogram or echocardiogram, may be necessary. These tests diagnose heart rhythm problems and to see how well your heart is pumping.
Heart failure is a chronic (lifelong) disease that requires ongoing management for the rest of your life. With aggressive treatment, the symptoms of heart failure can be drastically reduced. Medications and/or surgery can improve the symptoms and increase your likelihood of living longer. Lifestyle changes are also crucial, including quitting smoking or drinking alcohol. Patients should also maintain a healthy diet, lose weight or maintain an optimal weight, and get sufficient physical exercise.
The cornerstones of treatment are medications and lifestyle changes. Some of the medications used to treat heart failure include:
-
Angiotensin-converting enzyme inhibitors (ACEIs)/Angiotensin Receptors Blockers (ARBs) neutralize the effect of hormones that constrict blood vessels, increase fluid, and alter heart muscle proteins.
-
Angiotensin-receptor neprilysin inhibitors (ARNIs) is a combination medication that contains a neprilysin inhibitor and an ARB. Reducing the effect of neprilysin improves the opening of arteries and increases blood flow.
-
Beta Blockers block receptor sites of hormones that speed up the heart rate.
-
SGLT2-Inhibitors improve blood glucose control, help with weight loss, and decrease blood pressure.
-
Aldosterone Antagonists block sites of hormones that control how much sodium leaves the body through the urine. Decreasing absorption of sodium leads to a decrease in blood pressure and a reduction in fluid around the heart.
-
Digoxin may slow a fast heartbeat that has an abnormal rhythm and increase the force of contraction of the heart.
-
Hydralazine and isosorbide dinitrate are medications that widen blood vessels and allow more blood to flow through.
-
Diuretics increase urination allowing extra fluid and sodium to be eliminated from the body. This decreases the workload of the heart and decreases the buildup of fluid in the lungs and other parts of the body (ankles, legs).
-
Potassium and magnesium supplements may be needed to replace the losses of these minerals in the urine when taking diuretics.
-
Other medications may be prescribed for related conditions such as coronary artery disease, clot formation, irregular heart rhythms, and high cholesterol.
Surgical procedures may be used for heart failure, such as heart transplants or coronary bypass surgery, depending on the patient’s heart function and overall health.
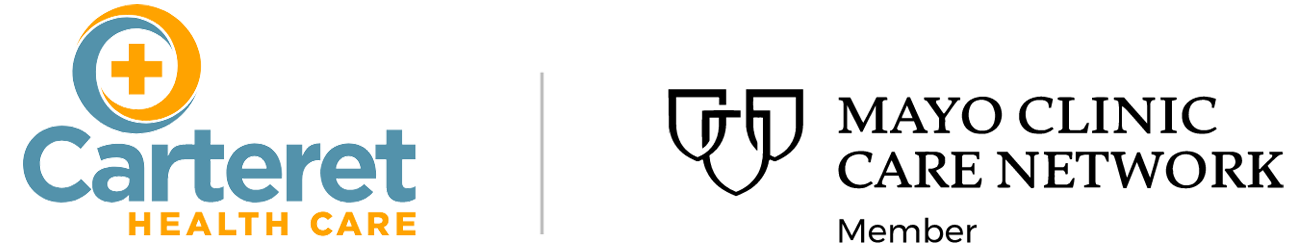
Download this Self-Check Plan for help with tracking your heart failure symptoms.
What Can I Expect?
The outlook for patients with heart failure continues to improve, and people can and do live with heart failure, even though it is a chronic disease. Because it is chronic (ongoing), you’ll be in treatment for heart failure for the rest of your life. Your doctor will prescribe a personalized program of medications and lifestyle changes and monitor your progress and adjust medications as needed.
A shift to low-sodium meals will be quite important! There is a wide selection of low sodium delicious meals that will help you make the change seamlessly.